How Interior Design Impacts Patient Experience in Medical Clinics
The way your clinic looks, feels, and functions shapes every part of a patient’s visit. From the car park to the consultation room, interior choices guide how people move, what they notice, and how safe and supported they feel. If you are planning a renovation and want a practical, healthcare‑specific approach to layouts and patient flow, you can see how we plan clinical spaces in our medical centre fitout projects for Australian practices.
Across Australia, clinic interiors benefit from trusted frameworks. Room planning and flows draw on the Australasian Health Facility Guidelines, building and access duties are grounded in the National Construction Code, general practice expectations are set out in the RACGP Standards for General Practices, and infection prevention guidance is provided by the NHMRC. Handling personal information in public areas is informed by the Office of the Australian Information Commissioner. Used with care, these references help create spaces that feel clear, calm, and clinically sound.
Why Interior Design Shapes Patient Perception and Trust
First Impressions and Emotional Safety
People often decide how they feel about a clinic within the first minute. Clear sightlines to reception, obvious check‑in cues, comfortable seating, and low background noise help visitors settle quickly. A simple sign hierarchy reinforces confidence, while glare‑free light and stable temperature reduce tension so conversations start on the right foot. Patient‑centred care guidance from the Australian Commission on Safety and Quality in Health Care highlights that environment influences confidence and communication in real, measurable ways.
Evidence‑Informed Design in Everyday Clinics
Evidence‑informed choices do not need to be complex. In practice, this means using well‑tested room proportions and flows from the AusHFG, aligning life‑safety, access and amenity with the NCC, and setting consultation norms against the RACGP Standards. These references help clinics design for comfort and clarity without guesswork.
Arrival and Entry: Setting a Calm, Confident Tone
Access and Approach for All Users
A good experience begins outside. A continuous accessible path from parking or public transport, intuitive entries, and even, safe lighting support independence and dignity. Australian accessibility expectations draw on AS 1428 and are applied through the NCC by certifiers; in Victoria this is overseen by the Victorian Building Authority. The Australian Human Rights Commission also reiterates that accessible environments are a right, not a bonus.
The Threshold: From Door to Reception
Stepping inside should feel intuitive. The entry should reveal where to go next, with a direct view to reception or clear direction to the check‑in point. Public wayfinding must sit beside mandatory emergency signage without cluttering it; the NCC determines emergency sign rules, which your visual system should complement, not overwhelm.
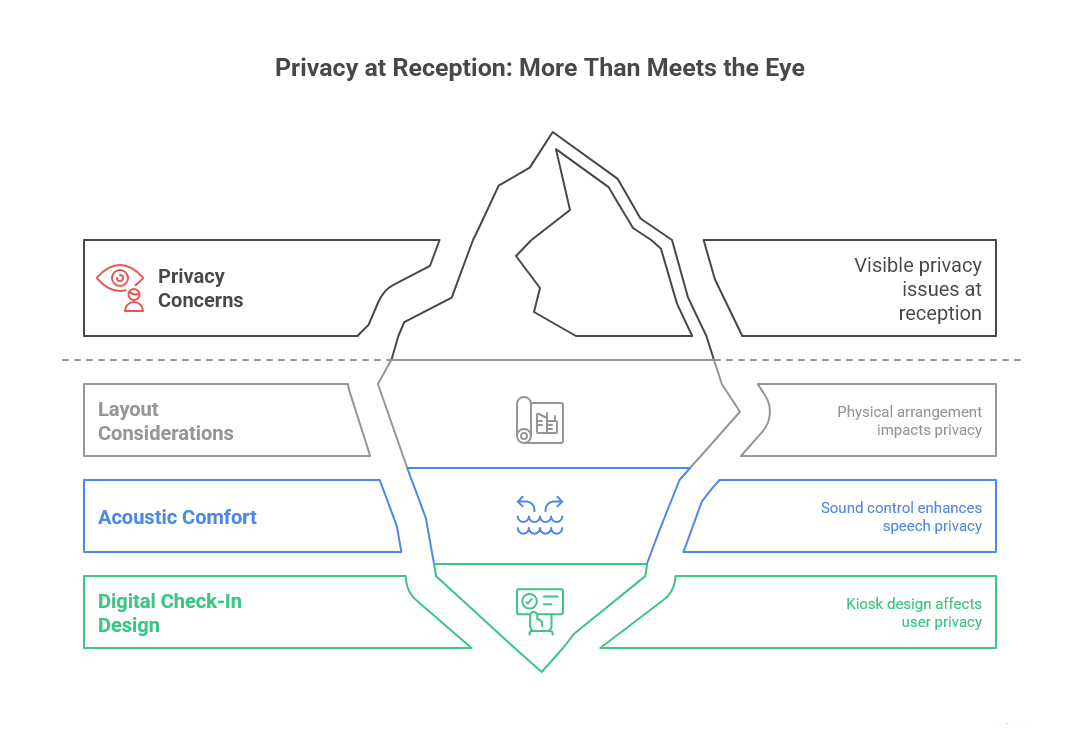
Reception and Check‑In: Privacy Without Barriers
Counter Design and Queue Behaviour
Reception is where privacy can falter if the layout is not considered. A lowered counter section integrated into the main desk supports equitable interaction without singling anyone out. Line‑of‑sight cues should keep queued visitors away from staff screens and conversations. These simple choices align with OAIC expectations for handling health information in public spaces.
Acoustic Comfort Around the Desk
Speech privacy at reception builds trust. Targeted acoustic absorption above and around the desk reduces conversation spill without changing the entire ceiling. Practical recommendations are available through the Australian Association of Acoustical Consultants, which publishes guidance on reverberation, background noise, and material selection for health environments.
Digital Check‑In That Feels Natural
Kiosks can help, but only when they are intuitive and positioned with care. Screens should be reachable for standing and seated users, with a clear route from check‑in to seating. Staff should be able to notice, from a distance, when someone needs help. And any on‑screen health information must be shielded from passers‑by, consistent with OAIC privacy guidance.
Waiting Areas: Comfort, Choice and Dignity
Seating That Serves Diverse Needs
Comfort is about choice and dignity. Provide a mix of seat types—some with arms, some without, varying heights and firmness—so people can choose what suits them. Integrate bariatric‑rated seating with the main arrangement rather than setting it aside. Keep routes clear for mobility aids and prams. The Consumers Health Forum of Australia notes that inclusive seating and clear movement paths reduce barriers and help patients feel respected.
Zoning for Different Energy Levels
Small zones can transform the experience. A low‑stimulus corner with softer lighting and fewer visual distractions helps people who are anxious or neurodiverse. Family clusters closer to reception can reduce wandering. A modest separation for symptomatic patients aligns with principles in the NHMRC infection prevention guidance without creating stigma.
Sensory Comfort: Light, Temperature and Sound
Layered lighting sets the foundation: warm ambient light with glare control, plus task light where needed. Guidance from the Illuminating Engineering Society of Australia and New Zealand supports comfortable lighting that still allows clear visual assessment. Thermal comfort should be steady and free of drafts; quiet ventilation aligned to good practice from AIRAH helps a space feel healthy rather than mechanical. For sound, reduce reverberation with selective absorption so speech is clear, calls are discreet, and background noise is not fatiguing; the AAAC provides useful targets for health facilities.
Consultation and Treatment Rooms: Respect and Communication
Eye Contact, Screen Sharing and Consent
Room layouts should support eye contact while making digital records easy to share. A monitor arm that swings toward the patient lets clinicians discuss results without breaking conversation. A companion chair positioned with clear sightlines to both clinician and patient helps with decision‑making and supports carers. The path from chair to bed should be short and free of obstacles so the movement feels natural.
Acoustic and Visual Privacy in Small Clinics
People need to feel certain that conversations stay in the room. Solid‑core doors with seals, partitions that run to structure (where feasible), and doors placed away from public sightlines work together to protect confidentiality. If corridor noise remains an issue, subtle sound masking can help. The Australian Acoustic Society provides guidance on approaches that avoid harsh finishes or an institutional feel.
Cleanability Without Feeling Clinical
Good detailing reduces risk and makes cleaning simpler. Continuous, coved floors in clinical rooms remove dirt traps at floor‑wall junctions; benchtops and junctions should avoid seams where possible. These principles align with the NHMRC infection prevention guidance. Warmth can still come through colour, pattern and art, so the room reads as clean and cared for rather than cold.
Telehealth‑Ready Rooms
Virtual care is now routine. A neutral backdrop, eye‑level camera, and front‑angled light reduce shadows and improve video clarity. A few soft surfaces can reduce echo. Reliable power and data with a little spare capacity helps rooms adapt as needs change. The RACGP and the Australian Digital Health Agency both offer practical resources for clinical telehealth setups.
Inclusive and Culturally Safe Interiors
Accessibility Beyond Minimums
Beyond minimum compliance is where a clinic starts to feel welcoming for everyone. Provide a continuous accessible path of travel to all key destinations, turning circles where needed, intuitive door hardware, and a reception counter with an integrated lowered section. High‑contrast signage and clear pictograms help people find their way. These choices reflect AHRC principles and are applied in Victoria by the VBA under the NCC.
Neurodiversity‑Aware Design
Predictable layouts, clear sightlines, reduced clutter, controlled glare, and low, even background noise support people with sensory sensitivities and reduce anxiety for many others. Simple visual schedules or signs that explain the steps in a visit can further lower stress.
Aboriginal and Torres Strait Islander Cultural Safety
Connections to Country and community can be expressed in meaningful, everyday ways. Locally relevant artwork, a visible Acknowledgement of Country, and clear, respectful wayfinding are small touches that signal welcome. Partnering with local groups during design aligns with the emphasis on consumer engagement promoted by the Department of Health Victoria.
Designing for Children and Older Adults
Children benefit from modest activity nooks visible from seating, with robust, wipeable finishes and calm colours. For older adults, seat height and armrests that support standing, good contrast at doorframes and steps, glare‑free light, and low background noise are practical helps. Guidance from the Australian Network on Disability and IESANZ can inform these decisions.
The Sensory Foundation: Light, Sound and Air
Daylight and Circadian‑Supportive Lighting
Daylight improves mood and orientation. Where windows are limited, tuned artificial lighting that provides adequate illuminance and suitable colour temperature throughout the day can support comfort and alertness. The IESANZ offers guidance that helps teams select appropriate sources and controls.
Acoustic Planning That Protects Conversations
Target low background noise and appropriate speech privacy, particularly around reception and consultation rooms. Place plant and noisy equipment away from quiet rooms where you can. The AAAC and Australian Acoustic Society both provide practical guidance for small health environments.
Air Quality Patients Can Feel
People notice stuffy or draughty rooms. Ventilation, filtration, and pressure relationships (where applicable) should support comfort and health without drawing attention to the engineering. The AIRAH provides guidance for selecting and operating systems, and the NHMRC links environmental controls with lower transmission risk in clinical settings.
Hygiene Signals That Build Trust
Hand Hygiene and Touchless Journeys
Place handrub dispensers at entries and in every treatment room where they are easy to see and use. Touchless taps, soap, and bins reduce contact points and make routines smoother. These are simple signals that align with Hand Hygiene Australia practice and the NHMRC infection prevention guidance.
Surfaces and Details That Stay Clean
Minimise seams and joints in clinical zones, select wipeable, durable fabrics, and detail door hardware and benchtop edges to avoid dirt traps. These details are small on paper but read very clearly to patients as signs of care and quality, consistent with NHMRC principles.
Technology That Supports Care (Not Screens That Dominate)
Patient‑Facing Tech That Reduces Stress
Queue updates and simple educational displays can reduce perceived waiting times when kept concise and readable. Keep personal details off public screens and handle data discreetly, consistent with OAIC expectations. Less, done well, often feels better than more screens everywhere.
Clinical Tech Integration
Keep cables tidy and out of traffic routes, use monitor arms for flexible positioning, and plan power and data with spare capacity for changes in devices. Guidance from the Australian Digital Health Agency can help align infrastructure with digital care workflows without making the room feel like a workstation first and a clinic second.
Data Privacy in Shared Areas
Simple moves like using screen privacy filters, placing terminals away from public sightlines, and providing a quiet spot for sensitive discussions all contribute to confidence. This is another area where practical steps flow from OAIC guidance.
Australian Standards and Guidance: What Patients Actually Feel
Translating the NCC and RACGP into Everyday Experience
Patients rarely notice compliance paperwork, but they do notice what it delivers—clear paths, accessible amenities, and confidence in safety. The NCC sets baseline life‑safety and access requirements, while the RACGP Standards address privacy, amenity and clinical norms. Viewed through a patient lens, these references explain why a clinic feels orderly and safe.
Using AusHFG as a Planning Lens
Many practices adapt elements from the AusHFG to guide room sizing, adjacencies and flows. That reference can help teams create logical journeys, with space for equipment and people to move without conflict.
NHMRC and AIRAH Together
Surfaces, cleaning routines and air systems work best when they are integrated. The NHMRC guides infection prevention decisions, while AIRAH offers advice on ventilation and filtration that supports health without making rooms feel mechanical.
Measuring What Patients Feel—and Improving It
PREMs and Quick Feedback Loops
Short environment questions—clarity, comfort, noise—help teams see what to adjust and in what order. The Department of Health Victoria encourages partnering with consumers; a QR code at the exit or a small tablet at reception can collect feedback without adding work for staff.
Post‑Occupancy Reviews and Small Wins
At 3, 6 and 12 months, look at where queues form, where people get lost, and which rooms feel too bright, cold or noisy. Modest changes—repositioned signs, different lamps, a window film, a few acoustic panels—can make the space markedly calmer. The Australian Health Design Council recommends using these reviews to tune the environment rather than waiting for a future refurbishment.
Staff Experience as a Patient Experience Lever
Staff who have good break spaces, ergonomic work points and simple workflows tend to engage more easily and warmly. The Australian Medical Association links staff wellbeing with care quality; investing in your team’s environment is a reliable way to lift patient experience.
Budget Priorities for a Calm, Clear Clinic
High‑Impact First Steps
Start where patients spend the most time. Layer the lighting and manage glare in reception and waiting, following IESANZ principles. Improve speech privacy around reception with targeted acoustic absorption, using guidance from the AAAC. Refresh seating diversity and clarify wayfinding. If your project touches multiple areas or mixes healthcare with other uses, we coordinate services, finishes and staging to reduce disruption across the site—see how we manage mixed scopes in our commercial projects.
Staging with Minimal Disruption
Swap lighting and seating after hours, and refresh treatment rooms one by one. Communicate what is changing and why—transparency turns disruption into a sign of care rather than an inconvenience. The Consumers Health Forum notes that clear, plain‑language updates support trust during improvements.
-
Focus on reception and waiting first. Layered lighting with good glare control, inclusive seating, and targeted acoustic absorption at the front desk tend to reduce stress immediately. These moves align with practical guidance from IESANZ on lighting balance and from the AAAC on managing reverberation and speech privacy.
-
-
Use the NCC for building safety and access, then align clinical norms with the RACGP Standards. Plan rooms and flows with references from the AusHFG, follow NHMRC guidance for infection prevention, and apply ventilation and filtration choices in line with AIRAH.
-
-
Use a short PREMs‑style survey with a handful of questions on clarity, comfort and noise, accessible via QR code or a small tablet at reception. The Department of Health Victoria promotes partnering with consumers; this is a practical way to adjust layouts, lighting or acoustics based on real‑time responses.