Healthcare Fitout: Designing Spaces That Enhance Patient Outcomes
The physical environment in which healthcare is delivered plays a profound role in patient outcomes, staff performance, and overall healthcare quality. From the moment a patient enters a healthcare facility, every aspect of the design—from layout and lighting to materials and acoustics—can either support or hinder the healing process.
For practice owners and those planning to establish healthcare facilities in Australia, understanding how to create spaces that actively contribute to positive patient outcomes is increasingly essential. As research continues to demonstrate the connection between physical environments and healthcare results, thoughtful fitout design has evolved from an aesthetic consideration to a strategic clinical priority.
This comprehensive guide explores the principles, elements, and implementation strategies for healthcare fitouts that enhance patient outcomes while meeting the unique operational needs of Australian healthcare practices.
The Science Behind Healthcare Design and Patient Outcomes
Evidence-Based Design in Healthcare Settings
Evidence-based design applies research findings to inform healthcare facility planning decisions. According to the Australian Institute of Health Innovation, healthcare environments designed using evidence-based principles can positively impact patient recovery times, medication requirements, and overall satisfaction with care.
Key research findings that inform healthcare design include:
Patients with access to natural light and views of nature typically experience shorter hospital stays and require less pain medication, according to studies documented by the Centre for Health Assets Australasia at UNSW.
Single-patient rooms reduce hospital-acquired infection rates by up to 45% compared to multi-bed wards, as reported by the Australian Commission on Safety and Quality in Health Care.
Appropriate acoustic design can improve patient sleep quality and reduce stress, with the Australian Acoustic Society noting that excessive noise in healthcare settings can increase blood pressure, heart rate, and stress hormones in both patients and staff.
Australian research has made significant contributions to this field. The Deeble Institute for Health Policy Research has documented how purpose-designed mental health facilities in Australia have reduced the use of seclusion and restraint by creating more therapeutic environments. Similarly, research from the University of Melbourne has demonstrated how thoughtful design of primary care settings can improve patient engagement and satisfaction with care.
These evidence-based approaches provide a scientific foundation for healthcare fitout decisions, moving beyond aesthetic preferences to design choices that measurably improve health outcomes.
Psychological Impacts of Healthcare Environments
The psychological effects of healthcare environments can significantly influence patient recovery and wellbeing. The Australian Psychology Society notes that healthcare settings often evoke anxiety and stress, which can interfere with healing processes and communication with healthcare providers.
Design elements that positively affect psychological wellbeing include:
Control and choice: Providing patients with options to adjust their environment (lighting, temperature, privacy) can reduce stress and increase satisfaction. The Australian Healthcare and Hospitals Association reports that patients who feel a sense of control over their environment typically experience less anxiety during healthcare visits.
Positive distractions: Thoughtfully selected artwork, nature elements, and entertainment options can redirect attention away from pain and anxiety. Research from the Arts Health Network Australia demonstrates that appropriate art in healthcare settings can reduce patient anxiety by up to 34%.
Social support spaces: Areas that comfortably accommodate family members or support persons help maintain important connections. The Consumers Health Forum of Australia emphasises that design that supports the presence of family can improve patient outcomes and satisfaction.
Different patient populations have varying psychological needs that should inform design decisions. The Royal Australian and New Zealand College of Psychiatrists provides guidelines for mental health facility design that emphasise safety while avoiding institutional appearances. Similarly, the Australian College of Rural and Remote Medicine notes that healthcare facilities serving Indigenous communities should incorporate culturally appropriate design elements that create welcoming, respectful environments.
Understanding these psychological factors allows practice owners to create environments that actively support mental wellbeing alongside physical health needs.
Staff Performance and Environmental Design
Healthcare environments affect not only patients but also the healthcare professionals who work within them. The Australian Medical Association reports that poorly designed workspaces contribute to burnout, reduced job satisfaction, and increased error rates among healthcare providers.
Research from the Australian Institute of Health and Welfare indicates that thoughtfully designed staff areas can:
Reduce physical strain and fatigue through ergonomic workstations and appropriate space planning
Decrease medication errors by up to 30% through well-designed medication preparation areas
Improve communication between team members through appropriate collaborative spaces
Reduce staff turnover by creating supportive work environments
The Australian Primary Health Care Nurses Association emphasises that nursing staff efficiency is directly affected by workspace design, with poorly planned facilities increasing walking distances, wasting time, and contributing to fatigue. Their guidelines recommend designing clinical spaces that minimise unnecessary movement while maintaining appropriate supervision capabilities.
Staff wellbeing features that support better patient care include:
Dedicated break areas that provide genuine respite from clinical work
Access to natural light and outdoor spaces during shifts
Appropriate acoustic management to reduce noise-related stress
Adequate storage and work surfaces to reduce clutter and improve efficiency
By recognising that staff performance directly impacts patient outcomes, practice owners can design environments that support their healthcare teams in delivering optimal care.
Key Elements of Effective Healthcare Fitouts
Spatial Planning and Patient Flow
Thoughtful spatial planning forms the foundation of effective healthcare environments. According to the Australasian Health Infrastructure Alliance, well-designed healthcare spaces should support clinical workflows while creating positive experiences for patients and visitors.
Key considerations for spatial planning include:
Logical sequencing of spaces: The patient journey should follow a natural progression from arrival through to departure, with clear pathways between related functions. The Australian Health Design Council recommends mapping typical patient journeys to inform spatial arrangements.
Appropriate adjacencies: Related functions should be located near each other to improve efficiency and reduce unnecessary movement. For example, treatment rooms should be easily accessible from consultation spaces, and diagnostic areas should have appropriate preparation spaces nearby.
Separation of public and clinical zones: Creating clear boundaries between public areas and clinical spaces helps maintain privacy, security, and infection control. The Royal Australian College of General Practitioners standards require appropriate separation between waiting areas and treatment zones.
Balancing privacy with observation requirements presents a particular challenge in healthcare design. The Australian Commission on Safety and Quality in Health Care recommends design solutions that maintain visual supervision where clinically necessary while preserving patient dignity. These may include partially glazed partitions, strategic staff positioning, and technology-enabled monitoring where appropriate.
Wayfinding systems help patients and visitors navigate healthcare environments confidently. The Australian Institute of Architects suggests using multiple cues to support navigation:
Clear, consistent signage using plain language and universal symbols
Architectural features that serve as landmarks and orientation points
Colour coding of different zones or departments
Digital wayfinding tools that complement physical elements
Effective spatial planning reduces stress for both patients and staff while improving operational efficiency—a critical consideration for practice owners seeking to optimise their healthcare facilities.
Material Selection for Healthcare Environments
Materials used in healthcare fitouts must balance infection control requirements with durability, maintenance needs, and aesthetic qualities. The National Health and Medical Research Council provides guidelines for environmental cleaning and infection prevention that influence material selection in healthcare settings.
Key infection control considerations include:
Surface cleanability: Materials should withstand regular cleaning with hospital-grade disinfectants without degradation. Non-porous surfaces are generally preferred in clinical areas.
Seam minimisation: Joins and seams can harbour pathogens and should be minimised, particularly in high-risk areas. Where seams are necessary, they should be sealed appropriately.
Antimicrobial properties: Some materials offer inherent or applied antimicrobial properties, though the Australian Commission on Safety and Quality in Health Care notes these should complement rather than replace regular cleaning protocols.
Durability is particularly important in healthcare settings, which typically experience heavy use and frequent cleaning. The Australian Building Codes Board recommends selecting materials based on their expected lifespan and performance under healthcare-specific conditions, including resistance to:
Impact and abrasion from equipment and furniture
Chemical exposure from cleaning products and disinfectants
Moisture in wet areas and high-humidity environments
UV exposure in areas with significant natural light
Balancing clinical requirements with aesthetic qualities creates environments that feel welcoming rather than institutional. The Design Institute of Australia suggests using materials that contribute to a healing atmosphere through:
Warm, natural textures in appropriate applications
Colour selections based on evidence about psychological responses
Patterns and finishes that reduce perceived institutionalism
Acoustic properties that contribute to a calming environment
A healthcare fitout that thoughtfully addresses material selection creates spaces that are not only safe and functional but also supportive of psychological wellbeing and positive patient experiences.
Lighting and Acoustic Design
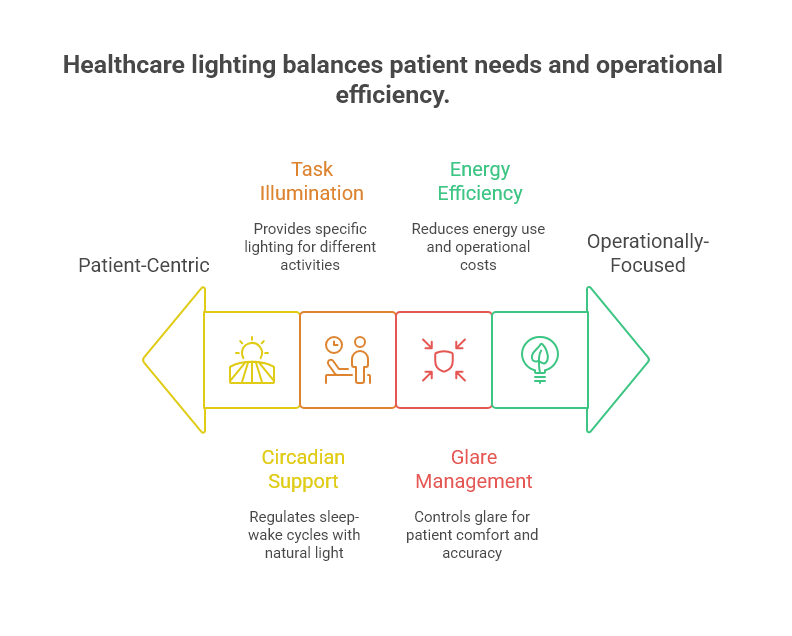
Lighting significantly impacts both patient outcomes and staff performance in healthcare settings. The Illuminating Engineering Society of Australia and New Zealand recommends healthcare-specific lighting strategies that address:
Circadian rhythm support: Lighting that mimics natural daylight patterns helps regulate sleep-wake cycles, particularly important in inpatient settings. Research from the Sleep Health Foundation indicates that appropriate lighting can improve patient sleep quality and reduce delirium in healthcare settings.
Task-appropriate illumination: Different healthcare activities require specific lighting levels and qualities. Clinical examination areas need high-quality, shadow-free lighting, while recovery spaces benefit from adjustable, warmer lighting options.
Glare management: Controlling glare is essential for patient comfort and accurate clinical observations. This includes managing both direct glare from light sources and reflected glare from surfaces.
Energy efficiency: The Green Building Council of Australia notes that lighting typically accounts for 20-30% of energy use in healthcare facilities, making efficient systems an important consideration for operational costs.
Acoustic design is equally important in healthcare environments. The Australian Association of Acoustical Consultants highlights several key considerations:
Speech privacy: Acoustic separation between consultation rooms and public areas is essential for confidentiality. The Office of the Australian Information Commissioner emphasises that protecting patient privacy includes preventing conversations from being overheard.
Noise reduction: Background noise can increase stress and interfere with communication. Sound-absorbing materials, strategic space planning, and equipment selection all contribute to quieter healthcare environments.
Sound masking: In some areas, appropriate background sound can help mask conversations and create acoustic privacy. The Australian Acoustic Society provides guidelines for effective sound masking in healthcare settings.
Creating appropriate sensory environments for different healthcare functions requires balancing these lighting and acoustic considerations with other sensory elements such as temperature, air quality, and visual stimulation. The Australian Healthcare and Hospitals Association recommends a holistic approach to sensory design that considers the specific needs of the patient population and clinical activities in each space.
Specialised Design Considerations for Different Healthcare Settings
Primary Care and GP Practices
General practice facilities have unique design requirements that support their role as community healthcare hubs. The Royal Australian College of General Practitioners Standards for General Practices outline minimum requirements for these facilities, but creating truly effective spaces goes beyond compliance to address workflow and patient experience.
Design elements that support general practice workflows include:
Flexible consultation rooms that accommodate various types of appointments, from brief consultations to minor procedures
Efficient clinical pathways that minimise staff travel distances between reception, consultation rooms, treatment areas, and support spaces
Appropriate storage solutions for the diverse equipment and supplies needed in primary care
Dedicated spaces for team collaboration that support the increasingly multidisciplinary nature of general practice
Creating welcoming, non-institutional environments is particularly important in primary care settings, which serve as many patients' main point of contact with the healthcare system. The Consumers Health Forum of Australia notes that patient-friendly environments can reduce anxiety and improve communication during consultations. Design strategies include:
Using residential-inspired design elements that feel familiar and comfortable
Incorporating local art or references to community identity
Providing clear information and orientation cues
Creating child-friendly spaces within waiting areas
Accommodating diverse patient needs requires thoughtful planning. The Australian Commission on Safety and Quality in Health Care emphasises the importance of designing for:
Cultural diversity through inclusive imagery and multilingual information
Age-appropriate spaces for both children and older adults
Accessibility beyond minimum compliance requirements
Privacy options for patients who may be distressed or unwell
Primary care facilities that address these considerations create environments that support both efficient healthcare delivery and positive patient experiences.
Allied Health and Therapy Spaces
Allied health services encompass a diverse range of therapies, each with specific spatial requirements. The Allied Health Professions Australia highlights the importance of designing spaces that support movement, rehabilitation, and specialised therapeutic interventions.
Designing for movement and rehabilitation involves:
Appropriate room sizing for activities requiring physical space, such as gait training or group therapy
Flooring selections that support safe movement while meeting infection control requirements
Supportive elements such as handrails, parallel bars, or ceiling tracks where needed
Visual privacy for patients during therapy sessions that may involve physical exposure
Equipment integration and storage solutions are particularly important in allied health settings, which often use a variety of therapeutic tools and devices. The Australian Physiotherapy Association recommends:
Dedicated storage for therapy equipment that is easily accessible but doesn't clutter clinical spaces
Flexible mounting systems for equipment that may need to be repositioned
Appropriate power and data access for electronic therapy equipment
Consideration of equipment pathways for large items that may need to be moved between spaces
Creating appropriate therapeutic environments involves addressing the sensory aspects of different allied health interventions. For example:
Speech pathology spaces benefit from excellent acoustics and minimal background noise
Occupational therapy areas need appropriate lighting for fine motor activities
Hydrotherapy spaces require specific temperature, humidity, and acoustic controls
Mental health therapy rooms need to create a sense of safety and containment
The Australian Health Practitioner Regulation Agency notes that allied health facilities must meet the specific standards of their respective professions while creating environments that support both clinical outcomes and positive patient experiences.
Mental Health and Wellbeing Facilities
Mental health facilities require particularly thoughtful design to create therapeutic environments that support recovery while ensuring safety. The Royal Australian and New Zealand College of Psychiatrists provides guidelines that emphasise the importance of design in mental health care outcomes.
Safety considerations in mental health design include:
Ligature-resistant fixtures and fittings in areas where patients may be at risk
Impact-resistant materials that can withstand potential damage
Appropriate observation capabilities that balance supervision with dignity
Safe outdoor access that provides connection to nature within secure boundaries
Creating calming, supportive environments involves attention to sensory aspects of design:
Visual calm through appropriate colour selection and minimal pattern
Acoustic comfort through sound absorption and noise control
Thermal comfort with individual control where possible
Connection to nature through views, natural materials, or therapeutic gardens
The National Mental Health Commission emphasises that mental health facilities should avoid institutional appearances while maintaining necessary safety features. Design strategies include:
Using residential-scale elements that feel familiar and comforting
Incorporating art and nature elements that provide positive distraction
Creating a variety of social spaces that support different levels of interaction
Providing sensory modulation spaces where patients can self-regulate
Balancing observation with dignity and privacy presents a particular challenge in mental health design. The Australian Commission on Safety and Quality in Health Care recommends design solutions that maintain necessary supervision while preserving patient dignity, such as thoughtfully positioned staff bases, appropriate use of technology, and careful planning of bedroom and bathroom layouts.
Mental health facility design that addresses these considerations creates environments that actively contribute to recovery and wellbeing rather than simply containing mental health services.
Technology Integration in Modern Healthcare Fitouts
Digital Infrastructure Planning
Healthcare facilities increasingly rely on digital systems to support clinical care, administration, and patient engagement. The Australian Digital Health Agency emphasises the importance of creating infrastructure that supports current needs while allowing for future technological advancement.
Key considerations for digital infrastructure planning include:
Network capacity and reliability: Healthcare facilities require robust networks that can handle clinical, administrative, and patient-facing systems simultaneously. The Australian Information Industry Association recommends designing networks with significant capacity beyond current needs to accommodate future growth.
Data security and privacy: Physical infrastructure must support cybersecurity requirements for healthcare data. The Office of the Australian Information Commissioner provides guidelines for protecting health information that influence server room design, cable pathways, and equipment placement.
Redundancy systems: Critical healthcare functions require backup systems to ensure continuity during power or network outages. The Australian Healthcare and Hospitals Association recommends redundant power and network connections for essential clinical systems.
Supporting telehealth and remote monitoring has become increasingly important in Australian healthcare. The Royal Australian College of General Practitioners telehealth guidelines suggest creating dedicated spaces for virtual consultations with:
Appropriate lighting that illuminates the provider without creating glare
High-quality audio equipment to ensure clear communication
Professional, neutral backgrounds that maintain a clinical appearance
Adequate soundproofing to ensure patient confidentiality
Future-proofing digital infrastructure involves creating flexible systems that can adapt to emerging technologies. The Australian Computer Society recommends designing easily accessible cable pathways, adequate power provision, and flexible mounting systems that can accommodate equipment changes without major renovation.
Equipment Planning and Integration
Medical equipment requirements significantly influence healthcare fitout design. The Medical Technology Association of Australia notes that equipment planning should begin early in the design process to ensure spaces properly support both current and future clinical needs.
Accommodating medical equipment involves addressing:
Spatial requirements: Equipment footprints, access needs, and clearances must be carefully considered. The Australasian Health Infrastructure Alliance provides guidelines for room sizes based on equipment types.
Structural support: Some equipment requires specific structural reinforcement or vibration isolation. The Australian Building Codes Board outlines structural requirements for different equipment types.
Services connections: Equipment may need specific electrical, data, water, gas, or ventilation services. The Standards Australia publishes technical standards for medical gas systems and other healthcare-specific services.
Radiation shielding: Imaging equipment may require lead lining or other radiation protection measures. The Australian Radiation Protection and Nuclear Safety Agency provides guidelines for radiation safety in healthcare facilities.
Flexible solutions for evolving technology help extend the useful life of healthcare fitouts. The Australian Health Design Council recommends:
Universal room designs that can accommodate different equipment types
Modular service delivery systems that can be reconfigured
Accessible ceiling and wall cavities for future service modifications
Generous sizing of electrical and data infrastructure
Balancing technology with human-centred care ensures that equipment integration supports rather than dominates the healthcare environment. The Australian Commission on Safety and Quality in Health Care emphasises that technology should enhance rather than replace human interaction in healthcare settings.
Smart Building Systems for Healthcare
Smart building technologies offer significant benefits for healthcare facilities, from improved patient comfort to operational efficiency. The Green Building Council of Australia notes that intelligent building systems can reduce energy consumption by 20-30% while creating better indoor environments.
Environmental control systems for patient comfort include:
Zoned HVAC systems that can adjust to different requirements in various clinical areas
Automated lighting controls that respond to occupancy and natural light levels
Individual control options that allow adjustment for patient preferences where appropriate
Air quality monitoring that ensures appropriate ventilation and filtration
Energy efficiency and sustainability technologies deliver both environmental and financial benefits. The Sustainability Victoria highlights several approaches particularly relevant to healthcare settings:
Heat recovery systems that capture waste heat from equipment
Smart metering to identify energy and water saving opportunities
Solar power systems to offset high healthcare energy demands
Water recycling systems for non-clinical applications
Monitoring and management systems help maintain optimal facility performance. The Facility Management Association of Australia recommends:
Building management systems that integrate multiple building functions
Preventative maintenance scheduling based on usage patterns
Remote monitoring capabilities for critical systems
Data analytics to identify efficiency improvement opportunities
These smart building approaches create healthcare environments that are not only more comfortable for patients and staff but also more cost-effective to operate—an important consideration for practice owners managing long-term operational costs.
Compliance and Standards in Australian Healthcare Design
Regulatory Framework for Healthcare Facilities
Healthcare facilities in Australia must comply with numerous regulations and standards that influence design decisions. The Australian Building Codes Board establishes baseline requirements through the National Construction Code, while healthcare-specific standards add additional layers of compliance.
Key regulatory considerations include:
Building Code of Australia (BCA) requirements for healthcare facilities, including fire safety, accessibility, and structural provisions.
Health facility licensing requirements, which vary by state and territory. The Australian Health Practitioner Regulation Agency notes that different healthcare services may have specific spatial requirements for registration.
Professional standards from bodies such as the Royal Australian College of General Practitioners, which include facility requirements for accreditation.
Work Health and Safety regulations from Safe Work Australia, establishing requirements for creating safe working environments for healthcare staff.
Accreditation requirements significantly impact healthcare facility design. The Australian Commission on Safety and Quality in Health Care National Safety and Quality Health Service Standards include several facility-related criteria, particularly around infection control, medication safety, and comprehensive care.
Navigating the approval process for healthcare facilities can be complex. The Australian Health Design Council recommends:
Early engagement with relevant authorities to identify all applicable requirements
Involving specialists familiar with healthcare compliance in the design team
Documenting compliance strategies throughout the design process
Building in contingency time for approval processes in project schedules
Understanding and addressing these regulatory requirements from the beginning of a healthcare fitout project helps avoid costly changes and delays later in the process.
Infection Control Requirements
Infection control considerations must be integrated throughout healthcare facility design. The National Health and Medical Research Council Australian Guidelines for the Prevention and Control of Infection in Healthcare provide comprehensive guidance that influences design decisions.
Design strategies for minimising infection risks include:
Appropriate hand hygiene facilities: The Hand Hygiene Australia program recommends strategic placement of handwashing stations and hand sanitiser dispensers throughout healthcare facilities.
Spatial separation: Creating appropriate separation between waiting patients, particularly those with potential infectious conditions. The Australasian Health Infrastructure Alliance provides guidelines for waiting area design that reduces cross-infection risks.
Air handling systems: Ventilation design that minimises airborne transmission risks through appropriate air exchange rates, filtration, and pressure relationships between spaces.
Clean and dirty workflows: Designing clear pathways for clean and contaminated items, including appropriate utility rooms for handling clinical waste.
Material and finish specifications for infection control should address:
Cleanability and resistance to hospital-grade disinfectants
Minimisation of joints and seams that can harbour pathogens
Appropriate use of antimicrobial surfaces in high-risk areas
Moisture resistance in areas with water exposure
Post-pandemic considerations have heightened awareness of infection control in all healthcare settings. The Australian Department of Health now recommends additional measures such as:
Increased spacing in waiting areas to allow physical distancing when required
Improved ventilation systems with higher air exchange rates
Touchless technology for doors, taps, and other high-touch surfaces
Flexible spaces that can be adapted during infectious disease outbreaks
Implementing these infection control measures within a welcoming, non-institutional environment requires thoughtful design that integrates technical requirements with patient experience considerations.
Accessibility and Inclusive Design
True accessibility in healthcare environments goes beyond minimum compliance to create spaces that work well for people of all abilities. The Australian Human Rights Commission emphasises that healthcare facilities must be accessible to people with disabilities under the Disability Discrimination Act.
Beyond minimum compliance, inclusive healthcare environments consider:
Diverse mobility needs: Providing clear pathways, appropriate turning spaces, and supportive features throughout the facility, not just in designated accessible areas.
Sensory considerations: Addressing the needs of people with visual or hearing impairments through appropriate lighting, acoustics, and wayfinding systems.
Cognitive accessibility: Creating intuitive layouts and clear communication systems that work for people with cognitive impairments or low literacy.
Size diversity: Accommodating larger patients with appropriate seating, doorway widths, and clinical equipment.
The Australian Network on Disability recommends designing healthcare facilities using universal design principles that benefit everyone, not just people with identified disabilities. These principles include:
Equitable use that works for people with diverse abilities
Flexibility in use that accommodates different preferences
Simple, intuitive operation of doors, fixtures, and equipment
Perceptible information provided through multiple sensory channels
Tolerance for error that minimises hazards and accidents
Low physical effort requirements for using facilities
Size and space appropriate for approach and use by anyone
Creating age-friendly healthcare spaces is particularly important as Australia's population ages. The National Ageing Research Institute provides guidelines for designing healthcare environments that support older adults, including:
Seating at appropriate heights with sturdy armrests
Good lighting without glare
Reduced background noise to support communication
Clear signage with good contrast and readable fonts
Flooring that reduces slip hazards and visual confusion
A commercial fitout approach that incorporates these inclusive design principles creates healthcare environments that truly welcome all patients, regardless of age or ability.
Implementation Strategies for Successful Healthcare Fitouts
Planning and Stakeholder Engagement
Successful healthcare fitouts begin with thorough planning and meaningful stakeholder engagement. The Australian Institute of Project Management emphasises that healthcare projects typically involve more stakeholders than many other building types, making engagement particularly important.
Involving clinical staff in the design process ensures spaces support actual work practices rather than theoretical workflows. The Australian Healthcare and Hospitals Association recommends:
Conducting workflow analysis with frontline staff
Using simulation exercises to test proposed layouts
Creating mock-ups of key spaces for staff evaluation
Establishing clinical reference groups for ongoing input
Patient input provides valuable perspectives that might otherwise be overlooked. The Consumers Health Forum of Australia suggests several approaches to gathering patient input:
Patient journey mapping to identify pain points in current facilities
Focus groups with diverse patient representatives
Surveys of existing patients about facility preferences
Inclusion of patient representatives on project committees
Experience mapping involves documenting the complete journey of different users through the facility, identifying opportunities to improve experiences through design. The Australian Health Design Council recommends mapping journeys for:
Different patient types with varying needs
Clinical and administrative staff
Visitors and support persons
Service providers such as cleaners and maintenance staff
Building consensus around design decisions helps ensure the finished facility meets stakeholder needs. The Australian Institute of Architects suggests using visual communication tools such as 3D renderings, virtual reality, and physical models to help stakeholders understand and evaluate design proposals.
Budgeting and Value Engineering
Developing realistic budgets for healthcare fitouts requires understanding their unique cost drivers. The Australian Institute of Quantity Surveyors notes that healthcare projects typically cost more per square metre than standard commercial fitouts due to:
Specialised infrastructure requirements
Higher specification finishes and systems
Complex services coordination
Stringent compliance requirements
Cost considerations specific to healthcare projects include:
Medical gas systems and specialised plumbing
Enhanced electrical infrastructure for medical equipment
Infection control measures in construction and materials
Specialised fixtures and fittings for clinical areas
Prioritising investments for maximum impact involves identifying which elements most significantly affect outcomes. The Australian Commission on Safety and Quality in Health Care suggests focusing resources on:
Elements that directly impact patient safety and clinical outcomes
Features that support staff efficiency and wellbeing
Areas where patients spend the most time
Systems that affect long-term operational costs
Long-term value versus initial cost considerations is particularly important in healthcare facilities, which typically have longer operational lifespans than many commercial spaces. The Green Building Council of Australia notes that investments in quality, durability, and sustainability often deliver significant returns over a facility's lifetime through:
Reduced maintenance and replacement costs
Lower energy and water consumption
Improved staff retention and reduced absenteeism
Enhanced patient satisfaction and loyalty
Value engineering in healthcare projects should focus on finding more cost-effective ways to achieve desired outcomes rather than simply eliminating features. The Australian Construction Industry Forum recommends collaborative value engineering workshops that bring together design, construction, and healthcare operational expertise.
Managing the Fitout Process
Healthcare fitout projects require careful management to ensure quality outcomes while minimising disruption to ongoing operations. For renovations of existing facilities, the Australian Medical Association recommends several strategies:
Staging works to allow continued operation of essential services
Creating temporary clinical spaces where necessary
Scheduling disruptive activities outside of operating hours
Establishing clear infection control protocols during construction
Maintaining clear communication with staff and patients about the process
Quality assurance throughout implementation is particularly important in healthcare projects, where defects can have serious consequences. The Australian Building Codes Board recommends:
Regular inspections by specialists familiar with healthcare requirements
Comprehensive testing of all building systems before occupation
Detailed documentation of compliance with all applicable standards
Formal commissioning processes for complex systems
Post-occupancy evaluation provides valuable insights into how well the completed facility meets its objectives. The Australian Health Design Council suggests conducting evaluations 6-12 months after occupation to:
Assess how spaces are actually being used
Identify any operational issues that need addressing
Document lessons learned for future projects
Measure outcomes against project objectives
Continuous improvement based on post-occupancy findings helps optimise the facility over time. The Australian Healthcare and Hospitals Association recommends establishing processes for ongoing evaluation and adjustment of healthcare environments to respond to changing needs and emerging evidence.
Conclusion
Creating healthcare environments that enhance patient outcomes requires a thoughtful approach that balances clinical functionality, human experience, and operational efficiency. By understanding the science behind healthcare design, implementing key elements effectively, and addressing the specific needs of different healthcare settings, practice owners can create facilities that actively contribute to healing and wellbeing.
The investment in quality healthcare fitouts delivers returns through improved patient outcomes, enhanced staff satisfaction and retention, and greater operational efficiency. As research continues to demonstrate the profound impact of physical environments on healthcare delivery, thoughtful design has become not just an aesthetic consideration but a clinical and business imperative.
For practice owners and those planning new healthcare facilities in Australia, partnering with designers who understand both healthcare operations and evidence-based design principles ensures your investment creates spaces that truly support your clinical mission and business objectives.
-
Research from the Australian Institute of Health Innovation demonstrates that healthcare environments influence patient outcomes through multiple mechanisms. Physical environments affect physiological stress responses, with poorly designed spaces increasing cortisol levels and blood pressure. They impact infection rates through factors like air quality, surface materials, and spatial separation. Environmental elements also influence sleep quality, with appropriate lighting and acoustic design improving rest and recovery. Additionally, well-designed spaces support better communication between patients and providers, leading to more accurate diagnoses and better treatment adherence. The Australian Commission on Safety and Quality in Health Care notes that these environmental factors can collectively impact length of stay, medication requirements, and overall treatment success.
-
According to the National Health and Medical Research Council, several design elements are critical for infection control in Australian healthcare facilities. Hand hygiene facilities should be strategically placed throughout the facility, including at entrances, in waiting areas, and in all clinical spaces. Material selection should prioritize non-porous surfaces that can withstand hospital-grade disinfectants without degradation. Ventilation systems need appropriate air exchange rates and filtration to reduce airborne transmission risks. The Australasian Health Infrastructure Alliance also emphasizes the importance of clear separation between clean and dirty workflows, including appropriate utility rooms for handling clinical waste. Post-pandemic, the Australian Department of Health recommends additional measures such as increased spacing in waiting areas and touchless technology for high-touch surfaces.
-
The Australian Digital Health Agency recommends approaching technology integration with the patient experience as the primary consideration. Technology should be visible and accessible when it benefits patients (such as self-check-in kiosks or information displays) but discreet when it might create barriers to human connection. The Australian Commission on Safety and Quality in Health Care suggests designing consultation rooms where screens can be easily shared with patients when discussing health information. Staff workstations should position technology to maintain eye contact with patients while accessing records. The Australian Healthcare and Hospitals Association emphasizes the importance of creating technology-free zones where human interaction is prioritized, particularly in mental health and palliative care settings. Additionally, providing adequate training for both staff and patients ensures technology enhances rather than hinders the care experience.
-
While initial costs for quality healthcare fitouts are higher than standard commercial projects, the Australian Medical Association notes that the return on investment manifests in several ways. Financially, well-designed facilities typically see improved operational efficiency, reduced staff turnover (saving recruitment and training costs), and increased patient retention and referrals. The Green Building Council of Australia reports that sustainable healthcare designs can reduce energy costs by 20-30% and water usage by 15-20% over the facility's lifetime. From a clinical perspective, the Australian Institute of Health Innovation has documented how evidence-based design can reduce medication errors, hospital-acquired infections, and length of stay—all of which have significant cost implications. Additionally, spaces designed with flexibility can adapt to changing healthcare needs without requiring complete renovation, extending the useful life of your investment.
-
The Australian Primary Health Care Nurses Association identifies several key design elements that support healthcare staff wellbeing. Ergonomic workstations reduce physical strain and injury risk, while thoughtful space planning minimizes unnecessary walking and improves workflow efficiency. Dedicated break areas that provide genuine respite from clinical work are essential, ideally with access to natural light and views. The Black Dog Institute emphasizes the importance of creating spaces where staff can decompress after difficult clinical encounters. Collaborative spaces support team-based care and reduce professional isolation. The Australian Healthcare and Hospitals Association notes that involving staff in design decisions increases ownership and satisfaction with the finished environment. Additionally, the Australian Medical Association recommends considering end-of-trip facilities for active commuters and adequate storage for personal belongings—small touches that significantly impact daily staff experience and long-term retention.